Abstract
Introduction
In many patients diagnosed with a hematological malignancy, the disease cannot be totally eradicated by conventional therapeutic approaches, and for them allogeneic hematopoietic stem cell transplantation (allo-HSCT) is the only curative option. A major complication of allo-HSCT is graft-versus-host disease (GvHD), affecting about 50% of transplant recipients. In addition to increased risk of death and long-lasting debilitating conditions, severe GvHD also impairs health-related quality of life. High-dose systemic steroids is the first line treatment for GvHD, but treatment failure is common, and steroid-refractoriness is a major cause of non-relapse mortality after allo-HSCT. While there is no established second line GvHD-treatment, extracorporeal photophoresis (ECP) has emerged as an attractive and increasingly applied alternative, partly due to its favourable safety profile. However, the use of ECP in preventing GvHD is sparse and data are inconclusive due to lack of randomized controlled trials (RCT). We therefore conducted a RCT to study if ECP given post transplantation could prevent the development of GvHD.
Methods
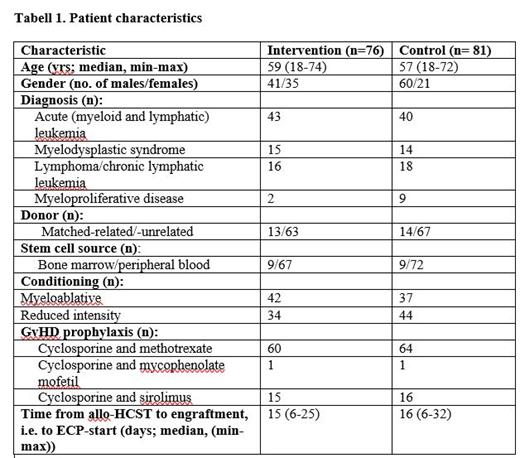
Between June 2017 and February 2020, we enrolled 157 patients (> 18 years) diagnosed with a hematological malignancy and treated with an allo-HSCT in first remission into an intention-to-treat open RCT. Ethical and IRB approvals were granted, and the RCT was registered with Clinical Trials (ID NCT03204721). The sample size (76 in intervention group and 81 controls) was calculated based on a reduction of 25% in the total number of patients diagnosed with any form of GvHD within the first year of allo-HCST (primary end-point) as clinically relevant. The patients were stratified according to whether they received myeloablative or reduced intensity conditioning (Table 1), and they were given GvHD prophylaxis as shown in Table 1. ECP (Therakos Cellex ®, Mallinckrodt Pharm., NJ) was initiated when patients had engrafted (i.e. leukocytes > 1 x 10 9/L and platelets > 20 x 10 9/L), and, according to the study protocol, we planned for ECP on two consecutive days/week for two weeks, then weekly for four weeks to a total eight treatments for each patient in the intervention group. Chi-square test was used to test differences between the two study groups.
Results
Table 1 shows that patient characteristics were well balanced among the two study groups. Four patients did not receive ECP while 39 received all the eight treatments. One year after allo-HCST, the proportion of GvHD was 45/76 (59%) in the intervention group and 52/81 (64%) in the controls (p=0.52). There were no significant differences between the intervention and control group regarding development of acute (45% vs. 48%) or chronic (39% vs. 40%) GvHD. Neither did we detect any statistical differences between the two study groups regarding organ involvement or severity of the GvHD manifestations (data not shown). During the one-year observation period, 16/76 (21%) and 10/81 (12%) relapsed in the intervention and control group, respectively (p=0.14). The corresponding numbers of deaths were 12/76 (16%) and 16/81 (20%), respectively (p=0.52). Six patients in the intervention group experienced mild to moderate temporary, adverse events that could possibly be related to the ECP-procedure.
Conclusion
In this first RCT addressing ECP as GvHD prophylaxis in allo-HSCT for hematological malignancy, we found no significant difference in the numbers, types, organ involvement, or severity of GvHD between the intervention and the control group. Thus, our study does not support the use of ECP as an adjunct to GvHD-prophylaxis based on cyclosporine and methotrexate, mycophenolate mofetil, or sirolimus. However, ECP did not seem to be harmful in this setting.
No relevant conflicts of interest to declare.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal